Pelvic Floor Therapy 101: Why It’s Not Just for Postpartum
For too long, the conversation around pelvic floor therapy has been relegated to a very specific milestone: “The Six-Week Checkup.” We have been conditioned to believe that the only time a woman needs to pay attention to the sling of muscles supporting her reproductive organs is after she has pushed a human being into the world.
But for women of color, particularly those navigating the complexities of uterine fibroids, endometriosis, and chronic pelvic pain, this narrow focus is a disservice. Your pelvic floor is the “basement” of your core. It is the foundation upon which your uterine health sits. And just as you wouldn’t ignore the foundation of your home until it collapsed, you shouldn’t wait for a major life event to care for your pelvic floor.
In this guide, we’re breaking down the walls. We’re moving beyond the “Kegel” and exploring why pelvic floor physical therapy (PFPT) is a vital tool for uterine health, symptom management, and reclaimed bodily autonomy.
What Exactly is the Pelvic Floor?
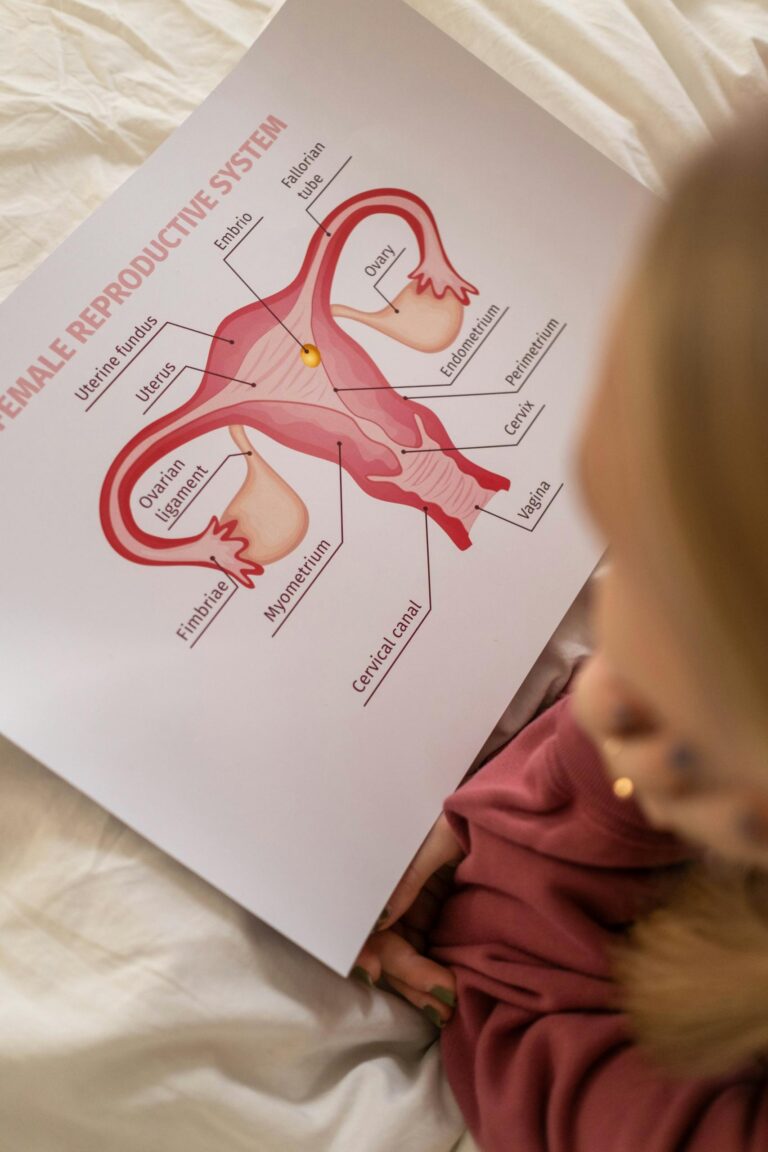
Before we dive into the benefits, we have to understand the anatomy. Imagine your pelvis as a sturdy bowl. The pelvic floor is a layer of muscles, ligaments, and connective tissues that stretch like a hammock from your pubic bone (in the front) to your tailbone (in the back).
This “hammock” has three primary jobs:
- Support: It holds your uterus, bladder, and bowel in place.
- Sphincteric: It controls the opening and closing of the urethra and rectum.
- Sexual & Reproductive: It plays a massive role in sexual response and the birthing process.
When these muscles are too weak (hypotonic) or too tight (hypertonic), the “bowl” doesn’t function correctly. For women with uterine conditions, the problem is often that these muscles are too tight—constantly bracing against pain.
The Uterine Connection: Why Your Uterus Needs Your Pelvic Floor
Uterine health and pelvic floor health are a feedback loop. When the uterus is in distress—due to fibroids, adenomyosis, or endometriosis—it sends distress signals to the surrounding muscles.
1. The “Bracing” Effect and Fibroids
If you are one of the 80% of Black women who will develop fibroids by age 50, you know the feeling of “heaviness.” Large fibroids can physically weigh down on the pelvic floor. In response, your pelvic muscles may chronically contract to “hold up” the extra weight. Over time, this constant contraction leads to muscle fatigue and trigger points.
PFPT helps by teaching these muscles how to release and lengthen, relieving that sensation of constant pressure and heaviness in the lower abdomen.
2. Endometriosis and Nerve Sensitivity
Endometriosis involves tissue similar to the uterine lining growing outside the uterus. This causes significant inflammation. When the pelvic floor is bathed in inflammatory markers, the nerves in the pelvis become “hypersensitized.” This means even a normal sensation (like a full bladder) can be interpreted by the brain as sharp pain.
A pelvic floor therapist works to “down-train” the nervous system. They use manual therapy to desensitize these nerve pathways, reducing the overall volume of your pain.
5 Benefits of Pelvic Floor Therapy for Uterine Health
I. Managing “Dyspareunia” (Painful Intercourse)
Pain during or after sex is a common, yet often silenced, symptom of uterine issues. Whether it’s deep pressure from a fibroid or sharp pain from endometrial lesions, the result is often “vaginismus”—where the pelvic floor muscles reflexively clamp shut in anticipation of pain.
How PFPT Helps: Therapists use dilators, manual release, and breathing techniques to teach the body that penetration does not have to equal pain. It’s about rewriting the muscle memory of your reproductive system.
II. Improving Circulation and Lymphatic Drainage
The uterus requires rich blood flow to function and heal. Chronic tension in the pelvic floor acts like a “kink in a garden hose,” restricting blood flow to the reproductive organs.
How PFPT Helps: Specific exercises and manual manipulations improve pelvic circulation. Better blood flow means more oxygen to the uterine tissues and more efficient removal of inflammatory waste products.
III. Alleviating “Endo Belly” and Digestive Distress
Many uterine conditions come with “Endo belly” (extreme bloating) or constipation. Because the pelvic floor muscles surround the rectum, tension in the “front” (the uterus) often leads to tension in the “back” (the bowel).
How PFPT Helps: Therapists teach visceral mobilization—a gentle massage of the internal organs—to help move gas and stool through the system, reducing the distension and bloating that makes uterine pain feel worse.
IV. Post-Surgical Recovery (Myomectomy & Hysterectomy)
If you have undergone surgery to remove fibroids or the uterus itself, you have scar tissue. Scar tissue (adhesions) is not flexible; it can pull on nearby organs and nerves, causing “phantom” pains years after surgery.
How PFPT Helps: Scar tissue mobilization is a cornerstone of therapy. A therapist can manually break up these adhesions, ensuring your internal tissues remain mobile and functional.
V. Bladder Control and Frequency
Ever feel like you have to pee every 30 minutes? Fibroids can press directly on the bladder, but often, the “urge” is actually caused by pelvic floor trigger points mimicking a full bladder.
How PFPT Helps: By releasing the tension in the muscles surrounding the bladder, you can often reduce the frequency and urgency of urination, even if you still have fibroids present.
Why the “Just Do Your Kegels” Advice is Often Wrong
If you go to a general practitioner and mention pelvic pain, they might tell you to “just do your Kegels.” For many women with uterine health issues, this is the worst possible advice.
If your pelvic floor is already “hypertonic” (too tight), doing Kegels is like taking a muscle that is already in a cramp and trying to lift weights with it. It will only increase your pain.
A Pelvic Floor PT will perform an assessment to see if you need to strengthen (contract) or lengthen (relax). Most women with chronic uterine pain need to learn how to relax their muscles first.
Overcoming the Barriers: Advocacy for Women of Color
We cannot talk about PFPT without talking about the “Care Gap.” Black women are less likely to be referred to pelvic floor specialists and more likely to have their pelvic pain dismissed as “normal” or “part of being a woman.”
How to Advocate for a Referral:
When speaking to your OBGYN, use specific, functional language. Instead of saying “it hurts,” try:
- “My pelvic pain is interfering with my ability to exercise/work.”
- “I am experiencing pain during intercourse that is impacting my quality of life.”
- “I would like a referral to a Pelvic Floor Physical Therapist to manage the muscular compensation from my fibroids.”
What to Expect at Your First Appointment
It is normal to feel nervous. A pelvic floor assessment is different from a standard pelvic exam.
- The History: They will ask about your period, your bathroom habits, your sexual health, and your birth history.
- The External Exam: They look at your posture, your hip mobility, and how you breathe. (Did you know that holding your breath can strain your pelvic floor?)
- The Internal Exam: With your consent, the therapist may use one gloved finger to gently palpate the muscles inside the vaginal canal to find “trigger points” or areas of tension. This is not a speculum exam. You are in control the entire time.
The Takeaway: Your Body is a System
Uterine health does not exist in a vacuum. Your uterus is cradled by muscles, fueled by blood vessels, and governed by nerves. When we treat the uterus but ignore the pelvic floor, we are only solving half of the puzzle.
Whether you are 22 and dealing with heavy periods, 35 and navigating fibroids, or 50 and entering menopause, pelvic floor therapy is a radical act of self-care. It is a way to stop “bracing” against your life and start living in your body again.
This information is educational and not medical advice. Consult a healthcare provider for diagnosis or treatment.