5 Ways to Tell if Your Period is Actually Normal

The menstrual cycle is often referred to by healthcare providers as the “fifth vital sign” (popularized by Lisa Hendrickson-Jack). Just like your pulse, blood pressure, temperature, and respiration rate, your period provides a monthly snapshot of your overall health. When something is off with your cycle, it is often the first indication that something is off with your endocrine system, your nutrition, your mental health, or your uterine health.
However, because menstruation is still frequently shrouded in “hush-hush” culture, many people grow up without a clear baseline of what is actually “normal.” We are often told that periods are “just supposed to hurt” or that being “irregular” is just a quirk of being a woman. This lack of clarity can lead to years of undiagnosed conditions.
Below is a comprehensive guide to understanding the boundaries of a healthy cycle and identifying the red flags that mean it’s time to stop “toughing it out” and start seeking answers.
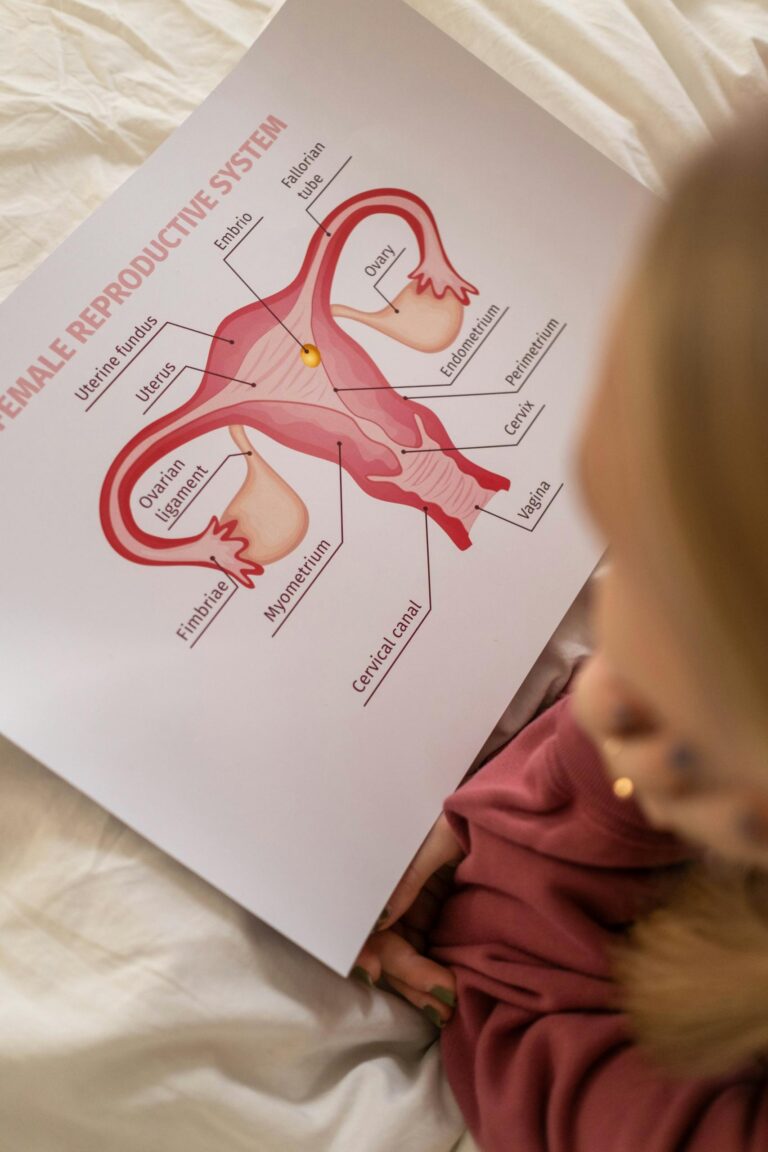
Part 1: The Anatomy of a “Normal” Period
While every body is different, clinical medicine (specifically the International Federation of Gynecology and Obstetrics, or FIGO) provides specific ranges for what constitutes a healthy menstrual cycle.
1. Frequency (Cycle Length)
Your cycle is measured from the first day of one period to the first day of the next, where normal is considered to be anywhere from 24 to 35 days.
- The Myth: The “28-day cycle” is an average, not a rule. If your cycle is consistently 25 days or consistently 35 days, you are likely within a healthy range.
2. Duration (Days of Bleeding)
This is the number of days you are actually shedding the uterine lining.
- Normal: Up to 2-7 days.
- The Myth: A “three-day period” is not too short, provided the flow is healthy. However, bleeding that stretches into day 9 or 10 is clinically considered “prolonged” and warrants investigation.
3. Volume (The Flow)
Flow is notoriously hard to measure, but clinicians generally look for a total loss of 5ml to 80ml per cycle.
- Normal: Changing a regular-absorbency pad or tampon every 3–4 hours.
- The Reality: Most people lose about 2–3 tablespoons of blood across their entire period. If you find yourself needing “super plus” products and changing them every hour, you are likely exceeding the 80ml threshold.
Part 2: Defining the “Abnormal” Period
Abnormal Uterine Bleeding (AUB) is a broad term used to describe any deviation from the patterns above. How do you identify if your cycle has shifted into the abnormal category?
Heavy Menstrual Bleeding (Menorrhagia)
Heavy bleeding is more than just an inconvenience; it can lead to chronic iron-deficiency anemia, which causes crushing fatigue and brain fog. You should consider your bleeding “abnormal” if:
- You soak through one or more pads or tampons every hour for several consecutive hours.
- You have to “double up” on products (e.g., wearing a tampon and a pad simultaneously to prevent leaking).
- You need to wake up in the middle of the night specifically to change your period products.
- You pass blood clots larger than a quarter (about 1 inch or 2.5cm in diameter).
Irregular Cycles
If you can never predict when your period is coming, your body may not be ovulating regularly.
- Polymenorrhea: Cycles that occur more frequently than every 21–24 days.
- Oligomenorrhea: Cycles that occur further apart than every 35 days.
- Metrorrhagia: Bleeding or “spotting” that occurs between your regular periods.
The Absence of a Period (Amenorrhea)
- Primary: If a person has not started their period by age 15.
- Secondary: If you have previously had regular periods but they suddenly stop for three months or more (and you are not pregnant, breastfeeding, or in menopause).
Part 3: The Pain Scale—When Is It Too Much?
Dysmenorrhea is the medical term for painful periods. There are two distinct types, and knowing the difference is vital for your diagnosis.
- Primary Dysmenorrhea: This is common cramping caused by prostaglandins (chemicals that make the uterus contract). It usually starts a day or two before your period and subsides by day three. It is generally manageable with over-the-counter anti-inflammatories or heat.
- Secondary Dysmenorrhea: This is pain caused by a structural or medical issue, such as endometriosis, fibroids, or adenomyosis.
Abnormal pain includes:
- Pain that does not respond to standard doses of Ibuprofen or Naproxen.
- Pain that forces you to miss work, school, or social commitments.
- Pain that occurs at other times of the month (like during ovulation or during/after sex).
- Pain accompanied by nausea, vomiting, or fainting.
Part 4: The “Why” Behind the Abnormalities
If your period is abnormal, it is rarely a random occurrence. It is usually a symptom of an underlying condition that requires specific management:
- PCOS (Polycystic Ovary Syndrome): Often causes very long, irregular cycles and may be accompanied by acne or excess hair growth.
- Uterine Fibroids: Benign growths in the muscular wall of the uterus that can cause extremely heavy bleeding and pelvic “heaviness.”
- Endometriosis: Tissue similar to the uterine lining grows outside the uterus, causing debilitating pain and potentially affecting fertility.
- Thyroid Disorders: Your thyroid and ovaries “talk” to each other. An overactive or underactive thyroid can make periods disappear or become dangerously heavy.
- Bleeding Disorders: About 20% of people with heavy periods since their first cycle actually have a mild underlying bleeding disorder like Von Willebrand disease.
Part 5: When to Seek Medical Attention
There is a difference between a “specialist visit” and an “emergency.” Knowing where to go can save your life—or at least your sanity.
Seek Emergency Care (A&E or ER) IF:
- The “One Pad an Hour” Rule: You are soaking through a high-absorbency pad or tampon every hour for two hours or more.
- Signs of Hemorrhage: You feel dizzy, lightheaded, or short of breath, or you actually faint.
- Sudden Severe Pain: Sharp, one-sided pelvic pain that comes on suddenly (this could indicate a ruptured ovarian cyst or an ectopic pregnancy).
- Fever: You have a high fever (over 101°F / 38.3°C) accompanied by pelvic pain or foul-smelling discharge.
Schedule a Specialist Appointment IF:
- Your cycles are consistently shorter than 24 days or longer than 35 days.
- You are spotting between periods or after sex.
- You have gone through menopause (no period for 12 months) and experience any amount of vaginal bleeding. Note: Post-menopausal bleeding is a red flag that must be investigated immediately to rule out cancer.
- You are passing large clots or your period lasts longer than 8 days.
How to Prepare for Your Appointment
Doctors rely heavily on data. Because your period only happens once a month, “guessing” from memory often leads to under-diagnosis.
- Track for 3 Months: Use a period tracking app or a simple paper diary. Note the start/end dates, the number of products used per day, and the size of any clots.
- Quantify Your Pain: Instead of saying “it hurts,” say “On day 2, my pain is an 8/10 and I cannot stand up for more than ten minutes.”
- Family History: Find out if your mother or sisters had heavy periods, fibroids, or early menopause. These conditions often have a genetic component.
Conclusion: You are the Expert on Your Body
The most important thing to remember is that you are the world’s leading expert on your own experience. If you feel like your period is controlling your life, or if you are constantly worried about “accidents” and “leaking,” that is not a normal way to live.
Do not let a provider dismiss your pain as “normal for a woman.” Use the clinical definitions provided here to advocate for yourself. Whether the answer is a simple hormone adjustment, a change in nutrition, or a surgical intervention for fibroids, you deserve a cycle that supports your life rather than disrupts it.
This information is educational and not medical advice. Consult a healthcare provider for diagnosis or treatment.